Home:
Meeting
Highlights: Posters
Home:
Meeting
Highlights: Posters

Management
of BI-RADS Category 5 Lesions: Usefulness of Fine-Needle Aspiration
Gal-Gombos EC, Esserman LE, Welsberry S, Recine MA and Poppifi RJ,
Jr.
OBJECTIVE:
The usage of
fine-needle aspiration (FNA) for accurate diagnosis of a breast
mass is declining when compared with core-needle biopsy. We analyzed
the utility of FNA as a quick and cost effective method in a special
group of patients who had mammographic lesions characterized as
highly suggestive of malignancy (BI-RADS category 5).
MATERIALS
AND METHODS:
Thirty-eight
patients underwent ultrasound guided fine needle aspiration of the
breast for 40 masses ranging in size from 0.6 to 4.1 cm. All the
masses were highly suggestive of malignancy on mammography (BI-RADS
category 5) and sonography. Nineteen of the masses were palpable.
The smears were evaluated for signs of malignancy. We reviewed FNA-s
and the corresponding histology of the breast masses.
RESULTS:
The FNA findings
were reviewed and compared to the surgical biopsy findings and in
all the cases the FNA was diagnostic. In our group of patients both
the specificity and sensitivity of FNA-s was 100%.
CONCLUSION:
FNA is an accurate
and efficient diagnostic tool. FNA can be the best diagnostic choice
in patients with BI-RADS category 5 lesions, with tumor status suggesting
no need for pre-surgery neoadjuvant therapy: 1) elderly, immobile
or non-compliant patients, who cannot rescheduled for an other day
for core biopsy 2) patients with coagulopathy or other contraindication
for large core needle biopsy.
Our objective
was to assess the potential clinical role for preoperative FNA in
the diagnostic evaluation of mammographically and or clinically
highly suspicious BI-RADS category 5 breast lesions. The usage of
fine needle aspiration for the diagnosis of a breast mass is declining
when compared with core needle biopsy. The reason is the easy use
of core biopsy, which is generally reproducible and provides a definitive
diagnosis in the majority of the cases. Another reason is that FNA
does not provide histological material, only cells. Carcinomas are
ideal lesions for cytopathologic examination since they are usually
very cellular.
The American
College of Radiology has developed the Breast Imaging Reporting
and Data System = BI-RADS, which is intended to standardize the
terminology, assessment of the findings and recommendation of action
to be taken. On the basis of the level of suspicion the mammographically
detected lesions can be placed into one of 4 categories (Category
1. means negative mammogram):
A.
Category 2.
B. Category 3.
C. Category 4.
D. Category 5. |
Benign
finding
Probably benign finding
Suspicious abnormality Highly suggestive of malignancy |
(Short
term follow-up)
(Biopsy should be considered) (Appropriate action should be
taken) |
A Category 5
lesion has a high positive predictive value (PPV) for carcinoma
(reported as 81-97 per cent). The features with the highest positive
predictive value--spiculated margins, irregular shape, linear morphology,
and segmental or linear distribution--warrant designation of a lesion
as category 5.
A consecutive
series of patients who presented with BI-RADS 5, underwent ultrasound
guided FNA from September to December 1999. The patient population
consisted of 38 women with 40 masses, mean age 70, and range 33
- 91 years.
The 38 patients
underwent ultrasound guided fine needle aspiration of the breast
for 40 masses ranging in size from 0.6 Š 4.1 cm in greatest dimension.
The patients
first underwent diagnostic mammogram and ultrasound and were found
to have BI-RADS category 5 lesions by at least two mammographers.
Only sonographically detectable lesions were included in this study.
FNA was performed by the standard technique. A high degree of accuracy
can be achieved with ultrasound guidance during the procedure. The
tip and long axis of the needle can be visualized with real time
sonography. Additional confirmation can be obtained by noting the
texture of the lesion upon entering it. Nineteen of the patients
had a palpable mass. The smears were evaluated for signs of malignancy.
FNA-s and the corresponding histology of the breast masses were
reviewed.
By using FNA
we diagnosed 39 of 39 carcinomas and the diagnosis for the one benign
lesion: fat necrosis was also suspected. The results were proven
by histology. In addition, FNA was able to demonstrate squamous
cells in a case of squamous cell carcinoma, mucin production in
two cases of mucinous carcinoma and indicated suspicion of lobular
morphology in one case of carcinoma.
The FNA findings
were reviewed and compared to surgical biopsy findings and in all
cases the FNA was diagnostic. In our group of patients both PPV
and sensitivity of FNA was 100%.
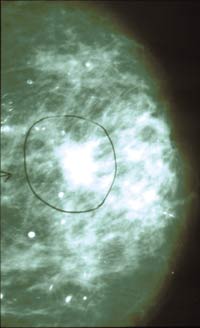
Figure
1. Infiltrating carcinoma, duct cell type. An 86-year-old patient
after left lower inner quadrant lumpectomy presents for routine
follow up.
1A. Right craniocaudal
mammography shows an irregular mass in the lateral aspect of the
left breast.
1B. Ultrasound demonstrates the 0.6cm mass.
1C. FNA shows highly cellular smears with carcinoma cells (Giemsa
x100).
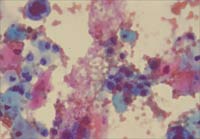
Figure
2. Squamous cell carcinoma. A 47-year-old patient presented for
screening mammography.
2A. Left mediolateral
mammography shows a BI-RADS 5 irregular mass.
2B. Sonography at the time of FNA. Irregular, hypodense mass with
the 18-gauge needle inside.
2C. FNA shows clusters and individual cells with abundant cytoplasm
and pink-orange keratinized squamous cells in the background (PAP
x200).
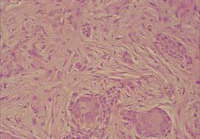
2D. Histopathology of the surgical excision showing the well-differentiated
squamous cell carcinoma (H and E x100).
|
FIGURE
1A
|
FIGURE
1B
|
|
|
|
|
FIGURE
1C
|
|
|
|
FIGURE
2A
|
FIGURE
2B
|
 |
 |
|
FIGURE
2C
|
FIGURE
2D
|
 |
 |
The wide use
of core biopsies in the USA has led to a decrease in the use of
FNA for diagnostic purposes. In addition, many surgeons donÕt trust
FNA for an accurate and definitive diagnosis. Our results support
our hypothesis that if there is a clinically and mammographically
highly suspicious BI-RADS 5 lesion and ultrasound guided FNA is
positive, no further biopsy is needed prior to surgery. If the FNA
is non-conclusive, with the above-mentioned clinical setting, another
procedure like core biopsy or surgical excision can be added. The
highest reported false negative rate for FNA have occurred with
the relatively paucicellular tubular and mucinous
carcinomas. Other types of infiltrating carcinomas are generally
very cellular and ideal for FNA diagnosis.
Figure
3. FNA shows a highly cellular smear with 3 dimensional clusters
of carcinoma cells (Giemsa x100). Histopathology (not shown) proved
infiltrating carcinoma, duct cell type.
Figure 4. FNA
shows single carcinoma cells in the background of mucin in a case
of mucin-producing breast carcinoma (Giemsa x100).
There are a
few lesions that can mimic carcinoma on mammography and sonography,
the most frequent is fat necrosis.
Figure
5. The diagnosis of fat necrosis (the only benign lesion) in the
presented series was suspected clinically because the 33 year-old
patient had a previous history of augmentation mammoplasty and the
lesion was superficial.
5A. FNA shows
multinucleated cells and pigment-laden macrophages and a few atypical
cells (Giemsa x400).
5B. Excisional
biopsy proved the suspected fat necrosis (H and E x10).
FNA has the
advantage of simplicity and shorter procedure time and is therefore
more cost effective than the other alternatives. We suggest using
core biopsy instead of FNA BI-RADS 5 lesions before neo-adjuvant
chemotherapy because a clip to locate the lesions can be put at
the same time as the biopsy procedure.
FNA is an accurate
and efficient diagnostic tool. It can be the best diagnostic choice
in certain patients with BI-RAD 5 lesions with tumor status suggesting
no need for pre-surgery neo-adjuvant chemotherapy such as:
|
FIGURE
3
|
FIGURE
4
|
|
|
|
|
FIGURE
5A
|
FIGURE
5B
|
|
|
|
Elderly, immobile
or non-compliant patients who cannot be easily rescheduled for another
day for a core biopsy or Patients with coagulopathy or other contraindication
for large core needle biopsy.
In addition
ultrasound guided FNA can be done the same time as diagnostic ultrasound,
eliminating the need for a time consuming and expensive second procedure.
1. Fornage
BD Sonographically guided needle biopsy of nonpalpable breast lesions.
J Clin Ultrasound 1999 Sep;27(7):385-98
2. Zardawi IM,
Hearnden F, Meyer P, Trevan B Ultrasound-guided fine needle aspiration
cytology of impalpable breast lesions in a rural setting. Comparison
of cytology with imaging and final outcome. Acta Cytol 1999 Mar-
Apr;43(2):163-8
3. Boerner S,
Fornage BD, Singletary E, Sneige N Ultrasound-guided fine-needle
aspiration (FNA) of nonpalpable breast lesions: a review of 1885
FNA cases using the National Cancer Institute-supported recommendations
on the uniform approach to breast FNA. Cancer 1999 Feb 25;87(1):19-24
4. Lister D,
Evans AJ, Burrell HC, Blamey RW, Wilson AR, Pinder SE, Ellis IO,
Elston CW, Kollias J The accuracy of breast ultrasound in the evaluation
of clinically benign discrete, symptomatic breast lumps. Clin Radiol
1998 Jul;53(7):490-2
5. Rubin M,
Horiuchi K, Joy N, Haun W, Read R, Ratzer E, Fenoglio M Use of fine
needle aspiration for solid breast lesions is accurate and cost-effective.
Am J Surg 1997 Dec;174(6):694-6; discussion 697-8
6. Sardanelli
F, Imperiale A, Zandrino F, Calabrese M, Bonifacio A, Canavese G,
Nicolo G Breast intraductal masses: US- guided fine-needle aspiration
after galactography. Radiology 1997 Jul;204(1):143-8
7. Greenberg
ML, Camaris C, Psarianos T, Ung OA, Lee WB Is there a role for fine-needle
aspiration in radial scar/complex sclerosing lesions of the breast?
Diagn Cytopathol 1997 Jun;16(6):537-42
8. Straathof
D, Yakimets WW, Mourad WA Fine-needle aspiration cytology of sarcomatoid
carcinoma of the breast: a cytologically overlooked neoplasm. Diagn
Cytopathol 1997 Mar;16(3):242-6
9. Meterissian
S, Fornage BD, Singletary SE Clinically occult breast carcinoma:
diagnostic approaches and role of axillary node dissection. Ann
Surg Oncol 1995 Jul;2(4):314-8
10. Phillips
G, McGuire L, Clowes D The value of ultrasound-guided fine needle
aspiration in the assessment of solid breast lumps. Australas Radiol
1994 Aug;38(3):187-92
11. Sneige N,
Fornage BD, Saleh G Ultrasound-guided fine-needle aspiration of
nonpalpable breast lesions. Cytologic and histologic findings. Am
J Clin Pathol 1994 Jul;102(1):98-101
12. Negri S,
Bonetti F, Capitanio A, Bonzanini M Preoperative diagnostic accuracy
of fine-needle aspiration in the management of breast lesions: comparison
of specificity and sensitivity with clinical examination, mammography,
echography, and thermography in 249 patients. Diagn Cytopathol 1994;11(1):4-8
13. Svensson
WE, Tohno E, Cosgrove DO, Powles TJ, al Murrani B, Jones AL Effects
of fine-needle aspiration on the US appearance of the breast. Radiology
1992 Dec;185(3):709-11
14. Evans WP
Fine-needle aspiration cytology and core biopsy of nonpalpable breast
lesions. Curr Opin Radiol 1992 Oct;4(5):130-8
15. Innes DJ
Jr, Feldman PS Comparison of diagnostic results obtained by fine
needle aspiration cytology and tru-cut or open biopsies. Acta Cytol
1983 May-Jun;27(3):350-4
Top
of Page
|