Melvin J Silverstein, MD |
EDITED COMMENTS |
 Estrogen receptor results and benefit from adjuvant tamoxifen in patients with DCIS Estrogen receptor results and benefit from adjuvant tamoxifen in patients with DCIS
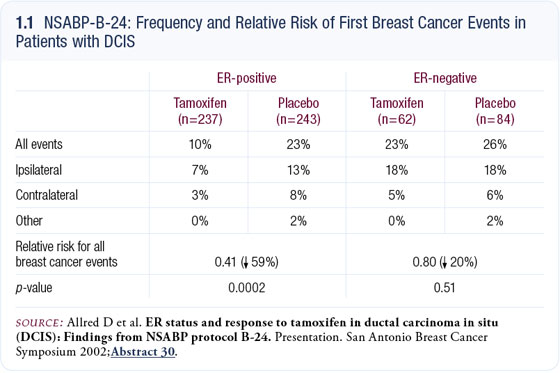
In NSABP-B-24, patients with DCIS had excision and radiation therapy and were randomly assigned to adjuvant tamoxifen or placebo. A statistical benefit in the local recurrence rate was observed for patients who received adjuvant tamoxifen (Fisher 1999).
Dr Craig Allred evaluated approximately 600 cases from NSABP-B-24. Patients with ER-positive disease derived benefit from treatment, whereas patients with ER-negative disease did not benefit (Allred 2002; [1.1]).
Role of adjuvant radiation therapy in older patients with small, ER-positive, node-negative, invasive tumors
The standard in the United States today is to treat invasive cancer conservatively with excision and radiation therapy. Two recent articles published in the New England Journal of Medicine — one from Canada by Dr Fyles and the other from Boston by Dr Hughes — evaluated women 50 years of age and older (Fyles 2004) and 70 years of age and older (Hughes 2004) who were randomly assigned to excision and tamoxifen with or without radiation therapy. Most of the patients had ER-positive, T1 (≤2 cm) tumors.
As expected, patients receiving radiation therapy had a lower local recurrence rate, but the absolute magnitude of that reduction was quite small. In Dr Hughes’ study, it was only three or four percent (Hughes 2004); in the Canadian study, it was seven or eight percent (Fyles 2004). Although the local recurrence rate was higher without radiation therapy, overall survival was identical for patients treated with or without radiation therapy.
Since those articles were published, I’ve treated a few women who were 65 to 75 years of age with well-excised, nonaggressive, ER-positive tumors. I showed those patients the literature, and they were interested. Two of them elected not to receive radiation therapy, and I think more patients with similar disease profiles will begin to consider declining radiation.
The alternative, however, might be to use MammoSite® radiation therapy, so you’re not withholding potentially life-saving radiation. Although I believe little difference will occur in survival, a significant difference will occur in local recurrence, which can be a very depressing, demoralizing event.
Image-detected breast cancer
I recently directed the Second International Consensus Conference on image-detected breast cancer. The first one was held in 2001 and was published in the Journal of the American College of Surgeons six months later (International Breast Cancer Consensus Conference 2001). At this recent second conference, the executive editor of the Journal of the American College of Surgeons was present, along with about 23 experts from all over the world. We discussed a variety of subjects: ductal carcinoma in situ, minimally invasive small tumors, minimally invasive breast biopsy and MRI.
Thirty years ago, image-detected lesions virtually did not exist. Almost all patients had palpable lesions, and more than half had positive nodes. For all practical purposes, DCIS did not exist. In 1978, the American College of Surgeons conducted a survey and found that less than one percent of all breast tumors were DCIS. Now, 25 to 30 years later, DCIS accounts for 21 percent of all the new breast cancer cases, of which 90 percent are nonpalpable and are detected mammographically.
The average size of an invasive breast cancer has decreased from about 3.5 to 4 centimeters 30 years ago to 10 to 15 millimeters today. We suddenly have tumors that we can’t feel in perfectly normal asymptomatic women without any physical findings. The abnormalities are almost always detected mammographically. Initially, in the 1980s and 1990s, all of these patients were taken to the operating room for an open wire-directed excision.
Today, I think that’s a bad idea. At the Second International Consensus Conference, we made a strong statement that the optimal way to biopsy this type of lesion is with a minimally invasive breast biopsy using an image-directed needle. The operating room should be reserved for definitive treatment, and we should attempt to subject patients to no more than one surgery.
Role of MRI in patients with breast cancer
At the Second International Consensus Conference on image-detected breast cancer, vigorous debate arose about the role of MRI. Without a doubt, this tool is coming of age. It was only of minor interest at the 2001 conference, and it was of tremendous interest at the 2005 conference.
Many uses for MRI are now accepted. For example, most patients who present with axillary metastases and an unknown primary lesion have breast cancer. Seventy to 80 percent of the time you’ll locate the primary tumor with an MRI, but not with any other tool. MRI is also valuable in evaluating patients with implants and in determining the extent of disease before and after neoadjuvant chemotherapy.
In every patient in whom I utilize a needle biopsy and mammography to diagnose infiltrating cancer, I try to follow up with an MRI. Many times the MRI will reveal more extensive disease in another quadrant or the other breast. A decision about what to do should not be based solely on the MRI. If disease is revealed elsewhere that precludes breast preservation, a biopsy should be performed and MRI-guided biopsy may be necessary. If the patient is adamant about saving her breast, histologic proof of disease somewhere other than in the breast is needed before committing the patient to a mastectomy.
Select publications
 |
Dr Silverstein is a Professor of Surgery and Henrietta C Lee Chair in Breast Cancer Research at USC-Keck School of Medicine and Director of the Harold E and Henrietta C Lee Breast Center at USC/Norris Comprehensive Cancer Center and Hospital in Los Angeles, California. |
|