| |
The rational decision at the moment is to consider tamoxifen still the gold standard. You have to recognize that there will be periods of uncertainty in the evolution of medicine and science. As it relates to the question of adjuvant anastrozole, we’re just going to have to live through this period of uncertainty.
— Michael Baum, MD, ChM, San Antonio, December 10, 2001
(Shortly after presenting the initial data from ATAC trial)
In the Lancet paper, which is being published this week simultaneously with Tony Howell’s presentation here in San Antonio, we now stick our necks out and say that anastrozole is the preferred initial treatment for postmenopausal women with hormone receptor-positive tumors.
— Michael Baum, MD, ChM, San Antonio, December 9, 2004 |
In 1983, I was a neophyte videographer in search of a compelling topic for my first CME extravaganza. As I scoured my mind for interesting ideas, I came across one that seemed to hold promise. Several years earlier, Chuck Vogel — a junior faculty member at the University of Miami — recruited me from my fellowship to join the breast cancer division of the Sylvester Comprehensive Cancer Center. Chuck always was and continues to be an “avid hormonalist,” and during my time working with him, he taught me to think about “hormones, hormones, hormones” whenever considering therapy for metastatic disease. With this background and perspective firmly in place, the unspectacular video, “Hormonal Therapy for the 1980s,” was born.
My initial aspirations for the video were quite high and with the help of the university’s “sophisticated” AV staff we managed to create a Pac-Man-like animation of an estrogen molecule scurrying into the cytoplasm where a magical union occurred with the relatively recently identified estrogen receptor. Tamoxifen was also illustrated as a competitive Pac-Man blocking this activity. For the video, I interviewed five women currently receiving hormone therapies, which included tamoxifen, megestrol acetate, Halotestin®, high-dose DES and an unpleasant but very effective agent called aminoglutethimide — a first-generation aromatase inhibitor.
At that point, tamoxifen was considered a kinder, gentler palliative therapy that the research-leader community believed would never have the curative potential of chemotherapy; however, one of the first clinical research leaders interviewed when I launched this audio series strongly contested that concept.
Michael Baum had conducted an adjuvant trial of tamoxifen in the United Kingdom, and in spite of the fact that patients with ER-negative and unknown tumors were included, the study demonstrated a disease-free and overall survival benefit for women receiving two years of therapy compared to control. Observers from the United States pretty much ignored Mike’s results, assuming some type of methodologic inferiority with European research. After all, how could a pill with a cytostatic mechanism of action change the natural history of the disease, particularly when so many other smaller trials had not shown an overall survival benefit?
This irritated the hell out of Mike, who realized that the other tamoxifen trials were underpowered to detect a survival difference. With that in mind, Mike, Craig Henderson, Richard Peto and others decided to put together an international meta-analysis of all trials of adjuvant systemic therapy, including tamoxifen. The hope was that there would be an adequate number of events (deaths) to evaluate the effect of these agents on survival. The initial results were presented at a closed meeting of investigators at Heathrow Airport a few months before the 1985 NIH Consensus Conference. Sure enough, with an adequate number of observed events, tamoxifen demonstrated a significant survival benefit in postmenopausal women with node-positive tumors. In an instant, adjuvant hormonal therapy had arrived.
The next overview documented benefit for patients with node-negative tumors, and later on, for premenopausal patients. Along the way, investigators noted an increased incidence of endometrial cancer, which severely sullied the previously untainted reputation of this fascinating agent. The state of California even declared tamoxifen a carcinogen. As tens of thousands of women were treated, the drug constantly battled an association with intolerable vasomotor symptoms and weight gain despite placebo-controlled data contrary to the latter.
In 1998, NSABP-P-1 — the Tamoxifen Prevention Trial — was unblinded and in a historic, nationally broadcast press conference, Bernie Fisher and colleagues fractured another oncologic paradigm. Surprisingly, physicians and patients seemed to ignore these findings. To this day, tamoxifen is uncommonly utilized for chemoprevention, except in women with known primary tumors.
During one of our “Meet The Professors” sessions at the recent San Antonio Breast Cancer Symposium, Richard Peto (now “Sir Richard”) discussed the dramatic decline in breast cancer mortality (about a third) in the United Kingdom and the United States over the last decade. When I asked Peto what he personally believed led to this encouraging trend, he responded with two words, “adjuvant tamoxifen.”
You can make a pretty good argument that this little pill has prevented more suffering from cancer than perhaps any other systemic agent in the history of oncologic therapy, and translational scientists like Craig Jordan and Kent Osborne have made important connections between clinical and laboratory observations that are leading to new treatment strategies. It also seems that the role of tamoxifen as first-line adjuvant endocrine therapy — at least for postmenopausal women — has been passed on to a new class of agents with important advantages in efficacy and tolerability.
The informal motto of our CME company is, “If it were easy, someone else would have already done it.” Being a pioneer is always a great challenge, and in oncology, tamoxifen boldly went where no agent had gone before, launching an era of molecular targeted therapy. Until that moment in 1985 when Peto ascended to the podium in Bethesda, no one could conceptualize that an essentially nontoxic oral agent could make such a difference in the biology of this often nasty and relentless disease. But it did, and anastrozole, letrozole, exemestane, fulvestrant and trastuzumab are now part of daily patient care in breast cancer, and other agents like bevacizumab and lapatinib stand in the wings.
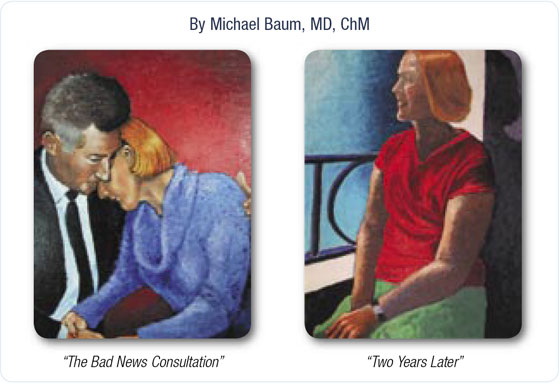
One of the reasons I enjoy chatting with Mike Baum so much is that he is a true renaissance oncologist. Like Corey Langer in lung cancer, Mike seeks to express his experiences and perceptions in art, and he shared with me two recent awardwinning oil paintings that capture the pain and healing of this challenging illness (see below). I believe Mike’s renderings are an apt representation of what happens in life to these patients and their families, and that the smiling and peaceful countenance so many women find a couple of years after the diagnosis of breast cancer is often the direct result of targeted agents like tamoxifen and the aromatase inhibitors. These agents quietly and usually innocuously prevent the disease from re-expressing itself, and allow patients to live healthier and longer lives.
— Neil Love, MD
NLove@ResearchToPractice.net
|
|

